Ambient pollution, both indoors and outdoors, and its impact on population health represent some of the most pressing environmental and public health challenges today. It is well established that the impact of air pollution on health is exceedingly high (Chen and Kan, 2008), although it ignores its real scope and effects on the aging process, since studies on air quality have largely focused on younger age groups. The World Health Organization (WHO) states that nine out of 10 people inhale air with elevated pollutant levels. Furthermore, the organization estimates that poor air quality is responsible for 7 million deaths annually (World Health Organization, 2021). In addition, household air pollution from the combustion of polluting fuel or inefficient stores also causes serious health effects, such as lung diseases, lung cancer, and cardiovascular diseases, and is believed to cause over 3 million deaths a year (WHO, 2024). Consequently, air pollution is recognized as a significant public health issue (Brugha and Grigg, 2014).
Road transport, agriculture, power plants, industry and homes are the largest emitters of air pollutants around the world (WHO). Particulate matter (PM) is a widespread and harmful air pollutants (Croze and Zimmer, 2018). PM originates from natural sources (dust, pollen, sea salt, and volcanic eruptions) and human activities (construction, fossil fuel combustion, and industrial processes) (López-Granero et al., 2024). It is also formed by chemical reactions in the atmosphere involving sulfur dioxide, nitrogen oxides, and ammonia, which are affected by temperature and humidity. Since the PM enters the body through the nose until it reaches the brain, the olfactory cortex is one of the main brain areas affected (Ranft et al., 2009; Ajmani et al., 2016). Some authors have demonstrated lower olfactory function in persons who live close to busy highways with heavy traffic (Ranft et al., 2009) and a positive relationship between increased exposure to PM and worse olfactory function (Ajmani et al., 2016) (Figure 1). Therefore, efforts are currently being made to understand the effects of anthropogenic PM derived from diesel vehicle emissions (Fonken et al., 2011). Furthermore, the effects they have on health are serious, due to ease with which they enter the respiratory tract and travel into the brain, making it especially vulnerable (López-Granero et al., 2024; Costa et al., 2019; Costa et al., 2021).
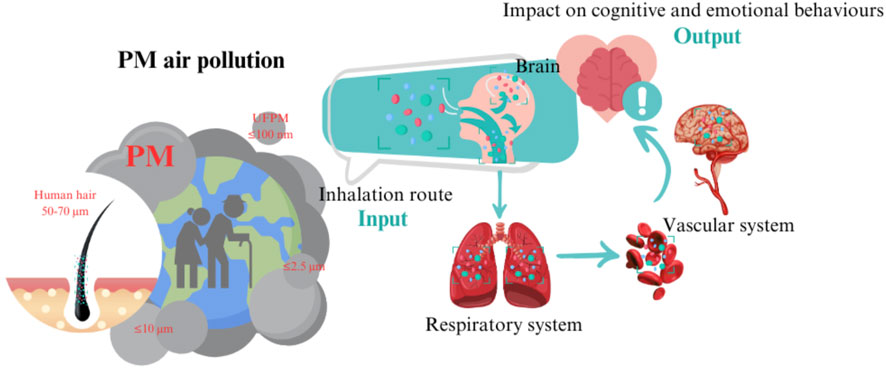
Figure 1. PM originates from a combination of natural and anthropogenic processes. These particles are capable of reaching the CNS and impacting cognitive and emotional functions, especially during aging. The route of access to PM is via inhalation through the nose. PM can (Chen and Kan, 2008) travel directly to the olfactory cortex and other brain regions or (World Health Organization, 2021) PM can be deposited in the lungs. Once it reaches the lungs, PM may also travel through the blood into the brain, causing brain disruption. Figure created with Canva.com.
PM is classified according to size: a) PM10: coarse particles ≤10 μm, mainly affecting the upper respiratory tract; b) PM2.5: fine particles ≤2.5 µm, capable of penetrating deep into the lungs and bloodstream; and c) ultrafine particles: <0.1 µm, with a high surface area to volume ratio, increasing their reactivity and health effects (Costa et al., 2021; Anderson et al., 2012). PM2.5, which is known to reduce visibility (haze), poses greater health risks than larger particles (EPA, 2025; Department for Environment and Food and Rural Affairs, 2025). Addressing these sources and properties is crucial for air quality management and public health protection. PM2.5 can remain in the air and travel hundreds or thousands of kilometers on air currents, exposing distant populations to pollutants. Studies have shown that long-range transport of PM2.5, spreads pollutants across regional and international boundaries (WHO, 2025). For example, PM2.5 from biomass burning, industrial activities, and traffic emissions can be carried by air currents, increasing pollution levels in downwind areas (Manousakas et al., 2021; Lucarelli et al., 2015; Zauli-Sajani et al., 2024; Lin et al., 2022). A study in northern South America found that aerosol transport increased local PM2.5 concentrations, increasing health risks such as cardiovascular and respiratory diseases (Velásquez-García et al., 2024). In Kyushu, Japan, researchers found that distant PM2.5 sources affected local air quality, highlighting the need for interregional cooperation (Kaneyasu et al., 2014). Similarly, a Mediterranean study found that long-range transport significantly affected PM2.5 levels, illustrating how atmospheric dynamics distribute pollutants (Perrone et al., 2013).
Many developed countries, including those in Europe, have failed to maintain urban air pollution levels below the WHO guidelines (World Health Organization, 2017). In 2021, the WHO established primary standards for PM2.5 at a 15 μg/m3 (24-h average) (WHO, 2023). This problem is illustrated by the fact that this value has been exceeded in many developed countries, surpassing WHO air quality guidelines despite stringent regulations. For instance, the U.S. frequently exceeds PM2.5 guidelines in areas like California’s Central Valley and Los Angeles due to vehicle emissions, industrial activity, and geographic factors trapping pollutants (World Health Organization, 2021). In the European Union, cities such as Paris, Milan, and Krakow report PM2.5 and NO2 levels above the WHO guidelines, driven by traffic congestion, industrial emissions, and solid fuel burning (World Health Organization, 2021). Despite its technological advancements, Japan experiences high ozone and PM2.5 levels in cities like Tokyo due to transboundary pollution and domestic industry (World Health Organization, 2021). These examples demonstrate that developed nations still face air quality challenges, requiring continued investment in clean energy, transportation, monitoring systems, and compliance with WHO’s 2021 guidelines (WHO guidelines and monitoring initiatives, accessed via https://www.iqair.com/newsroom/2021-WHO-air-quality-guidelines).
Numerous studies have shown that air pollution is associated with higher susceptibility to respiratory, cardiovascular, and cerebrovascular diseases (Clifford et al., 2016; Zhou et al., 2024) (Figure 1). However, its association with cognitive functioning and impairment requires additional study, as does its relationship with social and emotional status. Some studies have established a connection between air quality, specifically fine particles (PM2.5), and cognitive decline in older adults (Tallon et al., 2017). Evidence supports the link between poor air quality, cognitive impairment, and reduced successful aging (Cohen and Gerber, 2017). In fact, air pollution has also been associated with neurodegenerative disorders (Heusinkveld et al., 2016).
Given the potential health risks associated with environmental exposure like air pollution, these risks are particularly prevalent in urban areas due to gaseous pollutants and PM (Gatto et al., 2014). Thus, the connection between cognitive decline and exposure to neurotoxic ambient air pollution in urban areas (Gatto et al., 2014) is further reinforced by a series of studies published in recent years, which also highlight the relationship between urban environments and elevated levels of oxidative stress in the elderly (Sánchez-Rodríguez et al., 2006). Air quality appears to influence biological processes that directly affect cognition (Midouhas et al., 2018) and emotion (Lim et al., 2012; Power et al., 2015; Sass et al., 2017) by inducing neuroinflammation and oxidative stress (Block and Calderón-Garcidueñas, 2009; Calderón-Garcidueñas et al., 2004). Some studies have indicated that air pollutants can penetrate the blood-brain barrier, leading to systemic inflammation that negatively affects the central nervous system (Block and Calderón-Garcidueñas, 2009).
As mentioned, exposure to environmental pollution has been associated with a range of emotional alterations, such as depression, anxiety, and psychological stress (Lim et al., 2012; Power et al., 2015; Sass et al., 2017). Depression, the emotional factor that is most commonly associated with cognitive decline, has attracted significant academic attention. In geriatric populations, depression often co-occurs with measurable cognitive decline (Modrego and Ferrández, 2004; Rapp et al., 2011). Geriatric depression is considered a risk factor for Alzheimer’s disease (AD) (Rapp et al., 2011) and has been shown to increase the risk of dementia (Barnes et al., 2012; Ownby et al., 2006). Depression is also associated with cognitive decline and the onset of mild cognitive impairment (Feola et al., 2013; Wilson et al., 2014). However, these distinct pathologies are frequently confused (Dillon et al., 2014). Furthermore, a high prevalence of attention deficits has been linked to poor air quality (Siddique et al., 2011; Oudin et al., 2016; young and bok, 2017). Additionally, impaired autonomic and cognitive functions are predictors of impulsive-compulsive behavior at the time of a Parkinson’s disease (PD) diagnosis (Ricciardi et al., 2018).
According to several definitions, the process of human aging is complex and occurs in the biological, psychological and social spheres (Dziechciaż and Filip, 2014). A one-sided approach to aging would be incorrect. We raise the following question: Can air quality modulate cognitive, emotional, and social behaviors during aging? The aim of the present review was to deepen our understanding of behavioral consequence-dependent air quality during the aging process and the role of social health. In addition, it initiated a debate at the social and governmental levels regarding policies established by countries to address this public health issue.
2 The relevance of pollution-free residence for successful agingThe urban population is increasing rapidly worldwide. As cities expand, environmental quality, particularly urban air pollution, has become an increasingly critical factor in public health (Salim et al., 2013). Few studies have focused on identifying the predictive factors of cognitive decline in healthy elderly adults (Baumgart et al., 2015; Nguyen et al., 2002). Among these factors, there are variables centered on areas such as lifestyle and intellectual and social activities (Verghese et al., 2006). Following this argument, the Lancet Commission published a report adding new evidence to include pollution as a modifiable risk factor for dementia, including traumatic brain injury, high blood pressure, obesity, hearing loss, depression, diabetes, lower education, physical inactivity, smoking, alcohol abuse, social isolation, and pollution (Livingston et al., 2020).
It seems that the location of residence, whether rural or urban, and its inherent relation to environmental toxicity, pollution, and social conditions in these areas, could be considered as a predictive factor for healthy aging. Therefore, environmental pollution and the lack of socialization linked to urban environments deserve more attention in the study of risk factors of cognitive decline and emotional alterations (Gatto et al., 2014; Parra et al., 2022). In fact, some authors have already identified social relationships as a protective factor against aging (Tobiasz-Adamczyk and Zawisza, 2017). Tobiasz-Adanzczyk and Zawisza found an association between social activities and interactions and a better positive self-evaluation of health among elderly people living in rural environments in Poland (Tobiasz-Adamczyk and Zawisza, 2017). Furthermore, being married has been shown to be a protective factor against the effects of pollution, especially in the male population in South Korea (Kim et al., 2020).
Some studies have shown significant cognitive decline in relation to long-term exposure to urban pollution indices in different countries (Tan et al., 2023; Trushna et al., 2021; Weuve et al., 2012; Zeng et al., 2010; Zhang et al., 2024a; Tuffier et al., 2024). Air pollution is also associated with neurodegenerative conditions (Dimakakou et al., 2018; Shin et al., 2018; Yuchi et al., 2020). For example, it has been associated with a 2-year excess decline in cognitive function in relation to each 10 mg/m3 increase in long-term PM exposure in older women living in 11 US states, (Weuve et al., 2012). Other authors found similar results in women recruited from 24 states and Washington, DC, United States (Younan et al., 2022). In Brazil, Garbaccio et al. (2018) evaluated the quality of life of elderly people and concluded satisfactorily with good health in the cognitive processes of participants living in a rural Brazilian context. The favorable results derived from these studies merit discussion on a better redistribution of the population in favor of rural areas.
A consensus exists about the damage caused by pollution in urban areas in several cities worldwide (Gatto et al., 2014; Parra et al., 2022). However, other factors indirectly associated with air pollution exposure may contribute to the observed differences in cognitive abilities, such as socioeconomic status and emotional status. Exposure to environmental pollution is related to a range of symptoms such as depression, anxiety and psychological stress (Power et al., 2015; Lim et al., 2012; Sass et al., 2017; Tan et al., 2023; Trushna et al., 2021). Depression is also associated with cognitive decline and the incidence of mild cognitive impairment (Tan et al., 2023; Trushna et al., 2021; Tan et al., 2023; Trushna et al., 2021; Tan et al., 2023; Trushna et al., 2021; Tan et al., 2023; Trushna et al., 2021) and even geriatric depression has been considered a risk factor for AD (Rapp et al., 2011). These distinct pathologies are frequently confused in older adults (Dillon et al., 2014) (Figure 2).
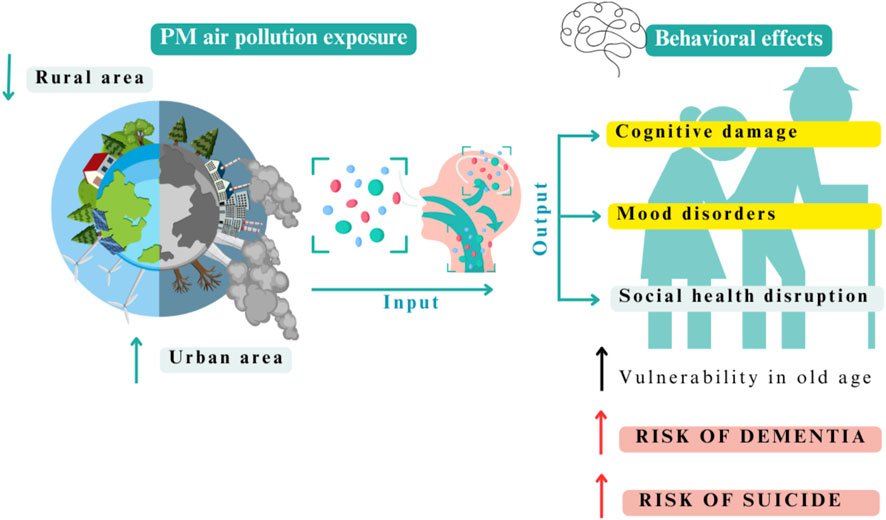
Figure 2. Overview of PM air pollution exposure and behavioral effects on human aging. In urban areas, the exposure to inhaled PM is high, leading to cognitive damage, mood disorders, and social health disruptions. The consequence is a higher vulnerability in older people with an increased risk of dementia and suicidal behavior. Figure created with Canva.com.
3 Air pollution and cognitive functioning in elderly peopleWith the rapid aging of the global population, it is estimated that this sector of the population increases annually between 12% and 22%, and within this group approximately 14% of adults aged 60 and over live with mental disorders (WHO, 2023). Air pollution is one of the factors associated with harmful effects on the central nervous system (CNS) is air pollution.
PM can reach other brain areas and cause cognitive dysfunctions (Table 1). Long-term exposure to PM2.5 has been shown to be strongly linked to impaired cognitive function in older Americans (exposure to PM2.5 also produces long-term mood disorders that have related pathways to affect as well cognition) (Tallon et al., 2017; Petkus et al., 2021). Inhalation of PM2.5 particles is associated with poor performance according to the Mini-Mental State Examination (MMSE) among the elderly in the US (Gatto et al., 2014; Parra et al., 2022), rural and suburban China (Ji et al., 2020; He et al., 2020; Wang et al., 2020) and Korea (Lee et al., 2022). Each 10 μg/m3 increase in exposure is estimated to be equivalent to two additional years of cognitive decline due to aging (Power et al., 2011). According to previous studies, a relationship between PM exposure and poor cognitive function (Cho et al., 2023; Ogurtsova et al., 2023; Kulick et al., 2020; Gui et al., 2024). A longitudinal study on aging in Taiwan (TLSA) established a relationship between exposure to PM with an aerodynamic diameter <10 μm (PM10) and cognitive impairment in older adult populations (Lo et al., 2019). This study demonstrated that co-exposure to ambient PM10 and O3 may deteriorate cognitive function to a greater extent in older adults. It is a fact that PM is able to damage the cognitive function by itself or along to others air pollutants such as O3 (Gatto et al., 2014; Gao et al., 2022).
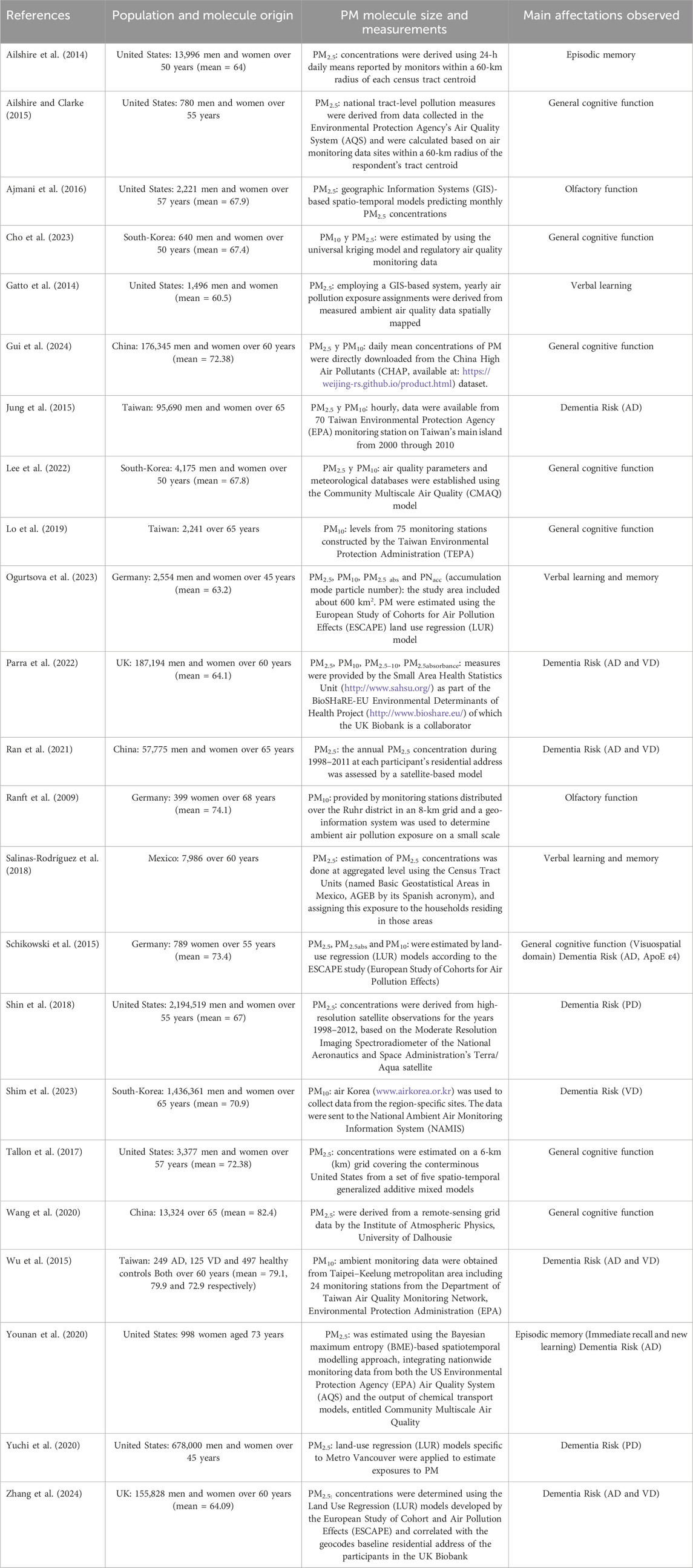
Table 1. Impact of PM exposure on older adults: key cognitive impairments and increased risk of dementia [Alzheimer’s Disease (AD), Parkinson’s Disease (PD), and Vascular Dementia (VD)] associated with PM exposure. Refer to Figure 6 for details on the geographical distribution.
Some studies have indicated that a specific cognitive subdomain is affected by PM exposure, not only by general cognitive status (Table 1). Specifically, in Germany, a study with a sample comprised of women older than 75 years indicated that those who lived near a busy road showed poorer performance in executive functions compared to those women who resided further from busy highways with heavy traffic (Ranft et al., 2009). Gatto and collaborators (2014) using a sample of 1,500 people with an average age of 60 years, found a reduction in verbal learning in US (Gatto et al., 2014; Parra et al., 2022). PM2.5 has also been found to strongly associate with a higher error rate on orientation and working memory tests in adults 55 years of age and older (Ailshire and Clarke, 2015) and reduced episodic memory compared to those with less exposure to PM2.5 (Younan et al., 2022; Ailshire and Crimmins, 2014). In addition, exposure to PM has been associated with lower scores on immediate verbal memory (Ogurtsova et al., 2023) and semantic verbal fluency (Salinas-Rodríguez et al., 2018).
Therefore, these studies have associated the exposure to PM with deficits in memory, working memory, episodic memory, verbal learning, memory, and attentional processes (Table 1) (López-Granero et al., 2024; Gatto et al., 2014; Ogurtsova et al., 2023; Younan et al., 2020; Yao et al., 2022a; Tonne et al., 2014; Wurth et al., 2018). It is noteworthy that working memory and attention are essential for normal cognitive development as well as being one of the first cognitive processes affected during aging. Working memory is a cognitive system that temporarily holds information for processing. Its function is crucial for any cognitive competence, such as learning, reasoning, problem solving and understanding language (Rivas et al., 2019; Vuontela et al., 2003). On the other hand, attention is a basic function required for higher cognitive abilities (e.g., executive function or memory) and involves different processes, such as selective attention to a particular source of stimulation or voluntary control (Anderson, 2002). Attention is also essential for controlling executive function. Inhibitory control deficits are characterized by the presence of impulsive behaviors, being a trait which appears to be present in various neuropsychopathological and neurodegenerative disorders (Robbins et al., 2012). It has also been indicated that poor cognitive performance and anxiety symptoms can predict the development of impulsive-compulsive behavior at the time of PD diagnosis (Ricciardi et al., 2018). In this sense, we highlight that the high prevalence of attention deficit has been associated with poor air quality in younger people (Tan et al., 2023; Trushna et al., 2021; Oudin et al., 2016; Young and Bok, 2017); however, it has not been studied in aging people, even when the interest in impulsivity is based on the theory that self-control could be related to measures related to longevity is currently on the rise (Strulik, 2019; Cohen and Gerber, 2017).
4 Air pollution and dementiaAccording to the WHO, the number of cases of dementia worldwide is increasing every 20 years by double the number of cases, taking into account the growth of the elderly population around the world (United Nations: World Urbanization Prospects, 2010), particularly in developing countries. In this regard, Figure 3 shows a comparative graph for increasing cases of AD and related dementias in Africa, America, Asia and Europe from 1990 to 2021. This graph shows how the number of years lived with disability (YLDs) in the population aged > 70 years in relation to AD and other dementias has increased over time. This trend is most prominent in regions of America, Asia, and Europe, with comparatively fewer cases reported in Africa.
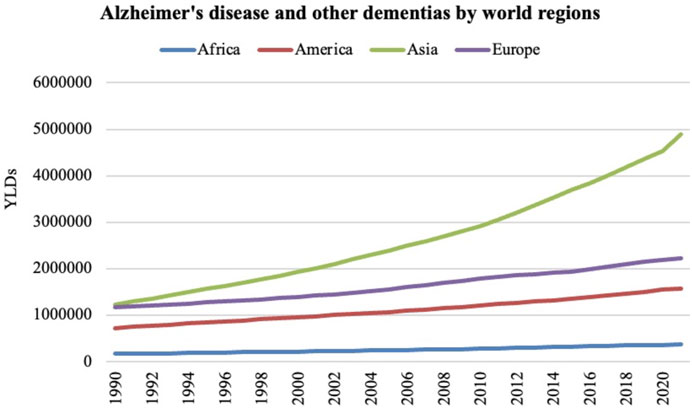
Figure 3. The number of years lived with disability (YLDs) in the population aged over 70 years in relation to AD and other dementias from 1990 to 2021 in Africa, America, Asia, and Europe. Institute for Health Metrics and Evaluation (IHME). GBD Compare Data Visualization. Global Burden of Disease (GBD) Study 2021. Seattle, WA: IHME, University of Washington, 2023. Available from http://vizhub.healthdata.org/gbd-compare. (Accessed 12/19/2024).
The 2017 Lancet Commission on Dementia Prevention, Intervention, and Care produced a list of possible risk factors for dementia including air pollution (Livingston et al., 2017). The 2018 Lancet Commission on Pollution states that a concurrent relationship is being built, specifically between fine PM and dementia in older people, thus requiring further research to examine emerging causal links (Landrigan et al., 2018).
In recent years, several human studies have demonstrated a link between air pollution exposure and dementia pathologies such as AD and PD (Table 1) (Costa et al., 2020; Mohammadzadeh et al., 2024; Peters et al., 2019). These findings raise the hypothesis that inhalation of particles (Calderón-Garcidueñas et al., 2004) negatively affects the brain, involving the activation of an inflammatory response and increasing production and deposition of Aβ peptides (Block and Calderón-Garcidueñas, 2009). A high incidence and risk of AD and PD dementias has been established for people exposed to PM ambient pollution and other air contaminants (such as NO2, CO, and O3 to name a few), around the world (e.g., Taiwan, Germany, Sweden, the United States, China and the UK) in the elderly (Parra et al., 2022; Braithwaite et al., 2019; Chang et al., 2014; Jung et al., 2015; Kasdagli et al., 2019; Schikowski et al., 2015; Wu et al., 2015; Ran et al., 2021; Wu et al., 2022). In a health and environment cohort study on a sample in the Ontario population (Chen et al., 2016) it was observed that exposure to PM2.5 was associated with a high incidence of dementia. In two other cohort studies involving 96,000 and 30,000 adults in Taiwan, exposure to PM2.5, was associated with a 54%–212% increase in the incidence of dementia (Chang et al., 2014; Jung et al., 2015). In another study carried out in the UK, positive associations were found between exposure to PM2.5, and the risk of all-cause dementia (Zhang et al., 2024b).
The social security coverage program administered by the United States government, which provides medical care to all people over 65 years of age known as Medicare, in one of the reviews of its users found data that for each increase of 1 μg/m3 at the annual concentration of PM2.5 citywide, there was an adjusted risk ratio (HR) of 1.08 for dementia (Kioumourtzoglou et al., 2016). Similar results have been found in other countries such as the UK, where samples from the UK Biobank were used to follow 155,828 elderly people aged 60 years and without a diagnosis of dementia for 12 years. Increases of 1 μg/m3 in ambient PM2.5 were found to have an adjusted hazard ratio (HR) of 1.07 for all-cause dementia risk (Zhang et al., 2024b). In general, it increases the risk of AD (Parra et al., 2022; Shim et al., 2023), PD (Shin et al., 2018; Yuchi et al., 2020) and vascular dementia (VD) (Parra et al., 2022; Shim et al., 2023) (Table 1).
Some authors have demonstrated an association between air pollution and respiratory and cardiovascular morbidity and mortality (Chen and Kan, 2008; Franchini and Mannucci, 2009; Ghio et al., 2012; Götschi et al., 2008; Pelucchi et al., 2009). VD is the second most common pathophysiological process (20%) after AD (Enhancing care, Advancing Health Science, 2025). Cardiovascular disease (CVD) is also known to affect cognitive function in later years (O’Brien, 2006; Rundek et al., 2022; Kalaria et al., 2016), and vascular and metabolic risk factors, including high blood pressure, obesity, diabetes, and stroke (Rosamond et al., 2008) are all inversely associated with cognitive function in middle-aged and older adults (Leritz et al., 2011).
It is worth mentioning that dementia and cognitive impairment, unlike cardiovascular disease, have no current treatment options (Livingston et al., 2020; Livingston et al., 2017) and should be considered an even higher risk to the population if the link between PM and cognitive decline is shown to be strong.
5 Air pollution and depression symptoms in elderly peopleA wealth of research shows that air pollution influences emotional responses such as happiness, anxiety, depression symptoms, life satisfaction, stress, sadness, pain, powerlessness, and nervous and mental disorders. These emotional responses to air pollution have been documented worldwide, including Australia, Europe, the United States, Latin America, Canada, and China (Altuğ et al., 2020; Barnett et al., 2018; Lu, 2020; Mendoza et al., 2019; Wang et al., 2019). One of the main emotional consequences of air pollution is depression or depressive symptoms, which have been increasingly observed in recent years. Figure 4 illustrates this rise in cases in Africa, America, Asia, and Europe from 1990 to 2021 among older adults. According to the World Health Organization (World Health Organization, 2017), depression is one of the most common mental health issues affecting more than 300 million people worldwide. A meta-analysis published in 2018 showed a statistically significant association between air pollution and depressive symptoms in older adults (Barnett et al., 2018) (Table 2).
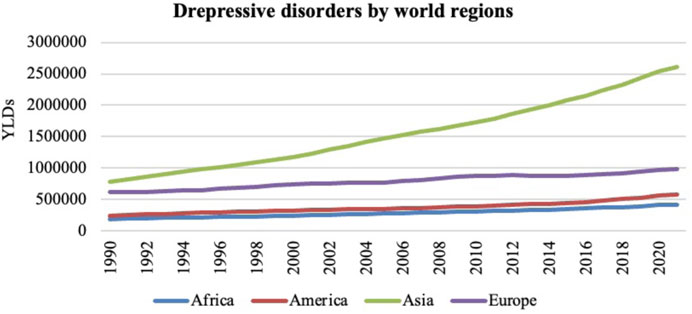
Figure 4. The number of years lived with disability (YLDs) in the population aged over 70 years in relation to depressive disorders from 1990 to 2021 in Africa, America, Asia and Europe. Institute for Health Metrics and Evaluation (IHME). GBD Compare Data Visualization. Global Burden of Disease (GBD) Study 2021. Seattle, WA: IHME, University of Washington, 2023. Available from http://vizhub.healthdata.org/gbd-compare. (Accessed 12/19/2024).
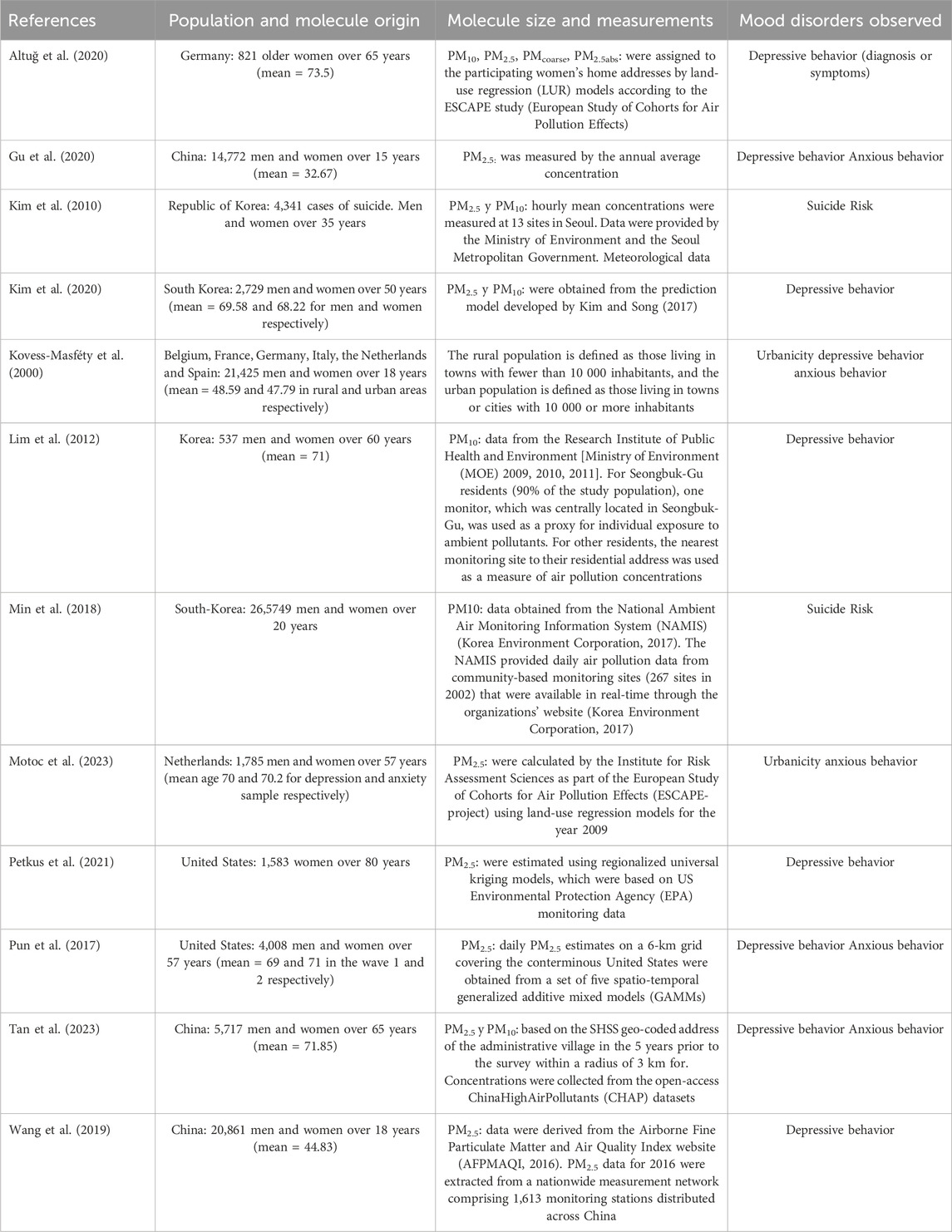
Table 2. Impact of PM exposure on older adults: key mood disorders associated with PM exposure. Refer to Figure 6 for details on the geographical distribution.
This association has been replicated in epidemiological and experimental studies with similar results. In 2019, Zhang and Wang (Zhang and Wang, 2019) found that high annual ground-level PM2.5 concentrations had significant negative effects on the average level of happiness in China with cross-sectional data. In addition to the Chinese population, some authors found that a higher concentration of PM2.5, significantly increased the prominence of the four negative emotions such as nervousness, depression, powerlessness, and restlessness (Gu et al., 2020). Additionally, Buoli et al. (2018) conducted a review with interesting results: long exposure to PM2.5 pollutant increased depressive symptoms (d effect size: 0.05–0.81 for each increase of 5–10 μg/m3 of air pollutant concentrations) (Buoli et al., 2018). Another review and meta-analysis study (Braithwaite et al., 2019) indicated that higher long-term exposure (>6 months) to PM2.5, was associated with higher odds of depression. Recently, some authors found that air pollution parameters, such as PM10 and PM2.5, were significantly and positively associated with depressive symptoms, even after adjustment for a German sample of elderly women (Altuğ et al., 2020). In addition, this study indicated that living within 100 m of a major road was positively associated with depression. Lim et al. (2012) conducted a study on elderly Chinese people and found that PM concentrations were significantly and positively related to depression. A systematic review and meta-analysis conducted in 2018 (Barnett et al., 2018) showed that air pollution, among other neighborhood characteristics, was positively related to depressive symptoms in the elderly population. This study evaluated a total of 73 articles with data from Asia, Europe, United States, and Oceania. Recently, two systematic reviews were published (Braithwaite et al., 2019; Cao et al., 2024). Both, which include a total of 22 and 25 papers, respectively, find associations between long-term exposure to PM2.5 and depression.
Overall, some of the aforementioned studies emphasized that the relationship between air pollution and mood disorders is remarkably different in rural and urban areas (Table 2). Similarly, Kovess-Masféty et al. also indicated that urbanicity seemed to be linked to a higher risk of mental health disorders, particularly depressive disorders (Kovess-Masféty et al., 2000). This finding is part of The European Study of the Epidemiology of Mental Disorders (ESEMeD 2000 study), which collected data from 6 European countries: Belgium, France, Germany, Italy, the Netherlands, and Spain. In Belgium, women in rural areas had fewer emotional disorders. Therefore, it seems that subjects living in metropolitan areas are more vulnerable to long-term PM10 exposure than those living in non-metropolitan areas (Young et al., 2018). It is worth mentioning that air pollution seems to trigger suicidal behavior; some authors have even indicated that air pollution exposure is associated with an increased risk of suicide in adults (Braithwaite et al., 2019; Young et al., 2018) (see Table 2). Kim and collaborators suggest that increased ambient PM associated to a higher suicide risk is more pronounced in persons 36–64 years of age (Enhancing care, Advancing Health Science, 2025). There are still insufficient studies that addressed the relationship between air pollution and suicide risk in the elderly.
In addition, it seems that air pollution contributes to depressive symptoms in older adults through feelings of loneliness (Zhang and Wang, 2019). Similarly, urbanicity was significantly associated with increased depressive symptoms, mediated by loneliness, physical activity, social support and air pollution (Pun et al., 2019). Social interactions seem to play a crucial role in shaping the overall quality of life of adults, particularly older adults (Scharf and Jong Gierveld, 2008; Bowling, 2005). Evidence indicates that limited or poor social connections can elevate the risk of dementia (Gardener et al., 2021). In addition, it has been shown that the probability of mortality increases by 30% in situations of loneliness, social isolation and living alone, so that, loneliness and isolation are considered predictors of physical, mental and psychosocial health problems in both rural and urban areas (Ibarra et al., 2020). Several studies underscore the advantages of aging in rural communities, such as robust social networks, enhanced social integration, and healthy and safe environments (Winterton and Warburton, 2012).
As well, depression is often associated with a decrease in overall wellbeing, affecting emotional, psychological, and social dimensions (Steptoe et al., 2015). Accordingly, air pollution may impair population health by influencing people’s subjective wellbeing (Li et al., 2019). Alternatively, as proposed by others, air pollution reduces subjective wellbeing by affecting physical health or reducing social contact with people outdoors, which indirectly affects subjective wellbeing (Zhang and Wang, 2019). In the study by Benavente Cuesta and Quevedo Aguadode (2019) on the Autoperception of Health, Quality of Life and Psychological Wellbeing among older people, a significant relationship was found between self-perception of health and the area in which people reside (rural and urban) (Benavente Cuesta and Quevedo Aguadode, 2019). The perception that the two groups have about their interpersonal relationships is attributed in this study to the phenomenon of depopulation experienced in rural areas in recent decades (Benavente Cuesta and Quevedo Aguadode, 2019).
6 Air pollution and anxiety emotion in elderly peopleThe effects of air pollution exposure on anxiety in older adults have not been well studied, despite the increasing diagnosis of anxiety disorders in the last 30 years around the world (see Figure 5). Negative emotions, such as nervousness, powerlessness, anxiety, and annoyance, have been linked to air pollution (Table 2). A few studies in the US have shown that an increase in PM2.5 is linked with anxiety symptoms, with the largest increase in the 180-day moving average during aging (Pun et al., 2017). In China, Tan and collaborators, in 2023 also found positive associations between exposure to PM2.5, PM10 and an increased prevalence of pain/discomfort and anxiety/depression mediated by higher socioeconomic status (affluent, urban, and higher level of education) (Tan et al., 2023).
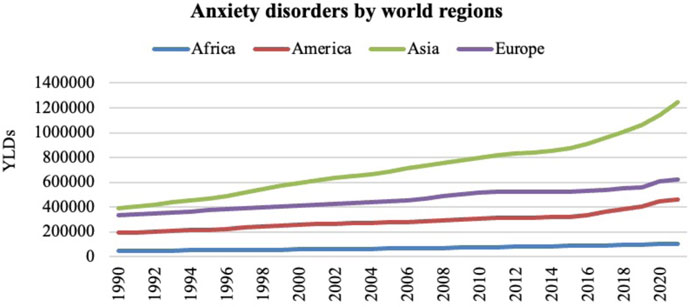
Figure 5. The number of years lived with disability (YLDs) in the population aged over 70 years in relation to anxiety disorders from 1990 to 2021 in Africa, America, Asia and Europe. Institute for Health Metrics and Evaluation (IHME). GBD Compare Data Visualization. Global Burden of Disease (GBD) Study 2021. Seattle, WA: IHME, University of Washington, 2023. Available from http://vizhub.healthdata.org/gbd-compare. (Accessed 12/19/2024).
A recent review (Lu, 2020) showed that exposure to PM2.5 in elderly women predicted increased anxiety symptoms. In addition, a systematic review and meta-analysis by Braithwaite team in 2019 reported significant positive associations between long-term exposure to PM2.5, and anxiety (Braithwaite et al., 2019). Higher concentrations of PM2.5, have been found to increase the negative emotions of nervousness and powerlessness in the Chinese population (Gu et al., 2020). Other works also found positive associations between air pollution and depressive and anxiety symptoms (Braithwaite et al., 2019; Zundel et al., 2022; Pun et al., 2017). Some authors have revised the literature and suggested that air pollution increases depressive and anxiety symptoms and behaviors, along with alterations in brain regions, leading to psychopathology risk (Zundel et al., 2022). The literature indicates that an increase in PM2.5 is significantly associated with anxiety symptoms, with the largest increase for the 180-day moving average in participants between 69 and 72 years old (Pun et al., 2017).
Neighborhood environmental characteristics play a relevant role in mental health during aging. Motoc et al. recently indicated that various neighborhood characteristics are associated with an increased incidence of anxiety, including higher urban density, higher PM2.5, and less green space (Motoc et al., 2023). Other studies have also found relationships between neighborhood characteristics and depressive or anxiety symptoms. For example, perceived social cohesion (Qin et al., 2023) and outdoor fitness facilities (Mu et al., 2023) are associated with a lower prevalence of depressive symptoms. These findings underscore the role of social characteristics in human health in the context of air pollution.
Social networks in the elderly may be sufficiently important to reduce the risk of mood disorders in older adults. In fact, Ward and colleagues found that greater social disconnection was associated with greater “wish to die,” with loneliness being the most important factor (Ward et al., 2024). Neighborhood is related to the services, accessibility, pollution, and social capital provided at the neighborhood level, and previous research has shown that it impacts both air quality and wellbeing (Lal et al., 2020). Similar to other emotional responses, Gu et al. (2020) suggested that exposure to a greater risk of air pollution might affect the mental health of the population by indirectly reducing wellbeing and social development. Thus, the concept of cognitive aging linked to brain toxicity secondary to environmental pollution in rural and urban areas does not explain the aging process in a global, unique, and direct way. A multidimensional vision is required that incorporates other factors associated with lifestyle, social support, and social networks in both areas.
7 Discussion and recommendations for future actionsSome studies have analyzed the role of residential settings and air pollution in the context of a behavioral frame in elderly people; however, they are insufficient. It seems that environmental agents could be the key to understanding the susceptibility and variability observed in behavioral symptoms during aging. The purpose of this review was to provide a deeper understanding of the cognitive, emotional, and social dimensions—both general and specific subdomains—which are influenced by air quality, place of residence, and individual susceptibility to environmental variations (Figure 2). Additionally, we highlight the role of social health and outline policy recommendations in the context of PM air pollution.
Aging is a universal phenomenon that does not necessarily have to bring the typical pattern of cognitive decline associated with dementia. Although we should note that cognitive decline is related to an increase in age, age is not a manipulated factor (Feldman and Kertesz, 2001; Kushwaha et al., 2017). Therefore, efforts should be directed to identify additional factors involved in the aging process, which could be susceptible to manipulation or variation. Might air quality be a key factor contributing to cognitive decline and mood disorders associated with aging?
7.1 PM air pollution associated with cognitive decline and mood disordersRegarding behavioral effects, Table 1 shows the main effects of air pollution exposure on cognitive function in elderly people. The number of cases of dementia worldwide is increasing along with the number of air pollutants and urban areas. The repercussions of air pollution on the brain and central nervous system imply cognitive alterations. It has been reported that the exposure to air pollutants cause a decrease in the cognitive function leading to moderate to severe damage (Tallon et al., 2017; Gatto et al., 2014; Petkus et al., 2021; Ji et al., 2020; Wang et al., 2020; Lee et al., 2022; Power et al., 2011; Cho et al., 2023; Gui et al., 2024; Lo et al., 2019; Tallon et al., 2017; Gatto et al., 2014; Petkus et al., 2021; Ji et al., 2020; Wang et al., 2020; Lee et al., 2022; Power et al., 2011; Cho et al., 2023; Gui et al., 2024; Lo et al., 2019; Tallon et al., 2017; Gatto et al., 2014; Petkus et al., 2021; Ji et al., 2020; Wang et al., 2020; Lee et al., 2022; Power et al., 2011; Cho et al., 2023; Gui et al., 2024; Lo et al., 2019; Tallon et al., 2017; Gatto et al., 2014; Petkus et al., 2021; Ji et al., 2020; Wang et al., 2020; Lee et al., 2022; Power et al., 2011; Cho et al., 2023; Gui et al., 2024; Lo et al., 2019). Several studies have observed notable cognitive declines associated with long-term exposure to urban pollution levels (Weuve et al., 2012; Zeng et al., 2010; Power et al., 2011). Some researchers have even reported a 2-year accelerated decline in cognitive function for every 10 mg/m3 increase in long-term PM exposure among older women (Weuve et al., 2012). Air pollution has also been linked to neurodegenerative disorders (Dimakakou et al., 2018; Costa et al., 2020). Specifically, the authors mark poorer performance in executive functions, lower olfactory function, deficits in working memory, episodic memory, verbal learning, attentional processes, impulsivity behavior and higher levels of mortality as the mains cognitive alterations (Ranft et al., 2009; Gatto et al., 2014; Siddique et al., 2011; Young and Bok, 2017; Ailshire and Clarke, 2015; Ailshire and Crimmins, 2014; Rivas et al., 2019; Sacks et al., 2011). On top of that, it seems that exist a higher incidence of dementia in cities with poor air quality (Costa et al., 2020; Braithwaite et al., 2019; Chang et al., 2014; Jung et al., 2015; Wu et al., 2015; Chen et al., 2016; Kioumourtzoglou et al., 2016). The authors specifically inform of higher risk of AD, PD and VD among the neurodegenerative diseases (Parra et al., 2022; Costa et al., 2020; Shim et al., 2023).
In addition, air quality is implicated in a range of emotional symptoms such as depression, anxiety and emotional wellbeing responses (Power et al., 2015; Lim et al., 2012; Sass et al., 2017; Altuğ et al., 2020; Barnett et al., 2018; Gu et al., 2020; Pun et al., 2017; Lu, 2020; Li and Zhou, 2020) (Table 2). Recent research has shown a positive association between air pollutants and depressive symptoms, even with a higher risk of suicidal behavior (Young et al., 2018). Moreover, older women seem to be more susceptible to developing depressive symptoms under air pollution conditions (Altuğ et al., 2020). Likewise, subjective environmental evaluations can modulate the link between objective environmental quality and life satisfaction by measuring feelings of wellbeing feeling (Li and Zhou, 2020; Liao et al., 2015). In general, these studies show a negative association between air pollution, life satisfaction, and happiness, indicating a negative impact of air pollution on emotional human responses. Some of these studies have shown that higher levels of air pollution, as well as living within 100 m of a major road, were significantly positively associated with emotional symptoms, foregrounding the relevance of residential settings (Altuğ et al., 2020).
7.2 Increased susceptibility to environmental pollution in older adultsSacks and colleagues established older adults as a vulnerable group to health effects related to PM exposure (Sacks et al., 2011). In addition, this research group was able to develop a definition of susceptibility that could be applied to include all populations potentially at risk of negative health effects due to air pollutant exposure. Aging is a natural process characterized by the gradual, time-dependent decline in biological and behavioral functions, with individuals of the same chronological age exhibiting variability (Sacks et al., 2011; Martins-De-Souza, 2023). Older adults are considered a susceptible population due to this gradual decline. Furthermore, older adults are considered more susceptible than younger groups because of the higher prevalence of preexisting cardiovascular and respiratory conditions, which may further increase their vulnerability to PM exposure (Sacks et al., 2011). With advancing age, studies on the dosimetry model of PM—which examines how these particles are deposited, accumulated, and cleared in different regions of the respiratory tract—have shown a reduced clearance of PM across all regions of the respiratory system (EPA, 2009).
So that, PM enters the respiratory tract via the nose to the olfactory bulb and travel into the brain, making it especially vulnerable (López-Granero et al., 2024; Costa et al., 2019; Costa et al., 2021). In fact, impaired olfactory function has been proposed as a precursor of AD (Calderon-Garciduenas et al., 1995; Fagundes et al., 2015). In this sense, some evidence also suggests an increased accumulation of amyloid-β in older individuals exposed to elevated levels of air pollution (Calderón-Garcidueñas et al., 2004). Therefore, PM pollutants may disrupt the blood-brain barrier and deposit in neural tissue, leading to systemic inflammation (Block et al., 2012). The inflammatory and oxidative stress responses triggered by air pollution are similar to those observed during natural aging, and the effects of these systems have been reported in the hypothesized biological pathways of neurological disorders (Dröge and Schipper, 2007; Schikowski and Altuğ, 2020).
Air pollution is not only associated with a higher susceptibility to respiratory and cerebrovascular systems but is also associated with CVD (Clifford et al., 2016; Zhou et al., 2024). Precisely, these systems show a decline with advancing age; therefore, environmental exposure could contribute to further deterioration. It has been reported increased cardiovascular disease hospital admissions among older adults compared with all ages when exposed to PM2.5 (Sacks et al., 2011; Pope et al., 2008). In this study, exacerbation of heart failure was associated with elderly patients, and the authors concluded that PM air pollution could be responsible for precipitating acute cardiac decompensation in otherwise well-managed patients with heart failure (Pope et al., 2008). A recent study observed that increasing exposure to PM2.5, was significantly associated with an increased risk of gastrointestinal bleeding, intracranial bleeding, and epistaxis in older adults (Fayyad et al., 2024).
7.3 The role of social health in mediating the effects of air pollutionThe role of social health in pollution-free residences in elderly people deserves to be discussed. Some authors (Blekesaune and Haugen, 2018) offered a specific view of the importance of treating the linkage between the elderly and the community to obtain a better quality of life. Many older adults living in rural municipalities reported a stronger sense of community than those living in urban municipalities (Verheij et al., 2008). Maintaining positive and lasting social relationships with friends and neighbors is essential for the quality of life of the elderly (Bowling, 2005; Scharf, 2001), and the neighborhood is a particularly important source of social contact for the elderly (Blekesaune and Haugen, 2018). Perceptions of who is considered a neighbor can vary be
Comments (0)