Export to PPT
Abstract Image
IntroductionCardiovascular disease (CVD) was considered to be a disease of men, but it is the leading cause of mortality in women globally.1 CVD remains less diagnosed and poorly treated among women2 possibly due to differences in clinical presentation. Endogenous estrogen has wide-ranging effects throughout the circulatory system in women. It increases high-density lipoprotein and decreases the low-density lipoprotein.3 There is a loss of estrogen effect after menopause and also it is stated that heart disease develops 7 to 10 years later in women than in men.3 4 Women's Heart Alliance in 2017 showed that 45% of women are unaware of CVD is the leading cause of death,5 which shows that awareness is much needed among women. Generally, the presentations of women with ACS differ compared with men as 37% of women with ACS reported no chest pain. Commonly reported symptoms are back, neck, or jaw pain.6 An unrecognized symptom leads to delay in treatment with a longer time from symptom onset to balloon, thrombolysis, or timely interventions. GUSTO IIb trial (Global Use of Strategies to Open Occluded Arteries in Acute Coronary Syndromes) showed that women with acute coronary syndrome (ACS) were older than men and have a high incidence of risk factors like diabetes mellitus (DM), hypertension (HTN), and dyslipidemia.7 The pathophysiology of ACS also differs among men and women. Plaque erosion due to endothelial dysfunction, toll-like receptor signaling, leukocyte activation, and modification of subendothelial matrix by endothelial or smooth muscle cells, trigger loss of adhesion to the extracellular matrix or endothelial apoptosis is the strong risk factors for ACS in women.8 The in-hospital mortality and morbidity are particularly higher in younger women than in man.9 10 The purpose of this study is to report a single-center experience in gender-based differences among patients undergoing percutaneous coronary intervention (PCI) and related outcomes.
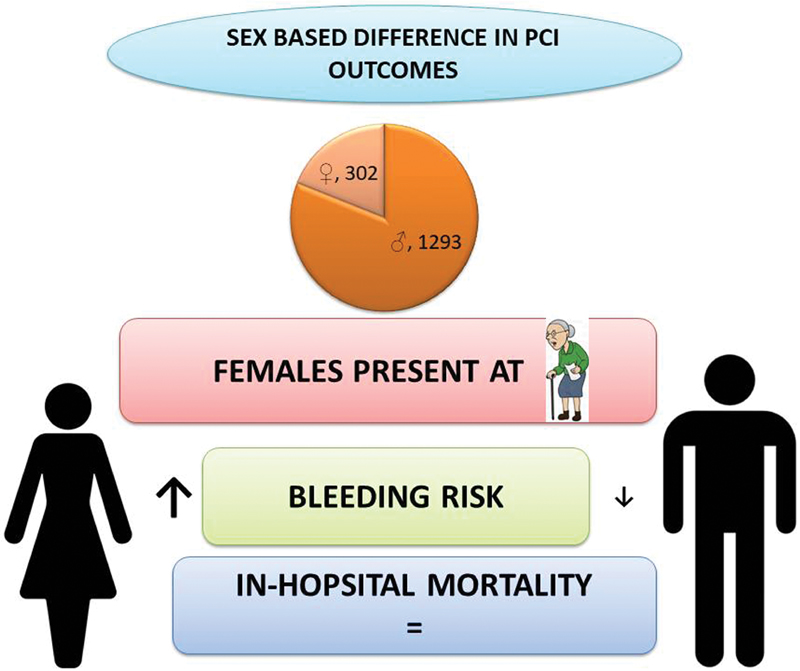
MethodsThis is a single-center, retrospective observational study. Consecutive patients who underwent PCI between January 2019 to December 2019 were enrolled in the study. A total of 1,595 patients underwent PCI in which 1,293 were males and 302 were females. Demographic characteristics, clinical and procedural details, and their in-hospital events were all collected. The primary outcome of the study is to assess the demographic, clinical, and angiographic characteristics of male and female groups who underwent PCI. The secondary objective is to analyze their clinical outcomes and major cardio and cerebrovascular events (MACE). The clinical events reported in this study include all-cause mortality, reinfarction, and hemorrhagic stroke, major bleeding, minor bleeding, target lesion failure, and repeat revascularizations. The MACE rate has been reported as a composite of death, reinfarction, and stroke. The definitions of the above-mentioned outcomes were provided in Appendix A and Appendix B.11 12 13
Statistical AnalysisContinuous variables were summarized using descriptive statistics and the categorical data are presented as numbers with percentages. Comparison of categorical variables between the two groups has been done with a chi-squared test. Comparison between two means was tested using two-tailed, unpaired t-tests for normal distribution and Mann–Whitney U test for non-normal distribution and is set at the statistical significance of 0.05. Statistical analysis was performed using SPSS 22.0
ResultsOverall, 1,595 patients were enrolled in the study in which 81.1% were males and 19% were females.
Table 1 shows the baseline clinical characteristics. Females presenting with symptoms were older than males (58 vs. 60.8 years, p < 0.001) and had higher body mass index (BMI) (26.2 ± 6.7 vs. 27.2 ± 4, p < 0.001). Risk factors like DM (57.8 vs. 69.5%, p < 0.001) and systemic HTN (50.2 vs. 65%, p < 0.001) were common in female. Smoking and alcohol consumption were reported high among males. Chronic kidney disease was more common in males (3.6 vs. 0.7%, p = 0.005). The clinical presentations were reported in Table 2. Females were more likely to present as unstable angina (16.2 vs. 22.7%, p-0.009) and they are less likely to get thrombolysed when presented with ST-elevation myocardial infarction (STEMI) (13.5 vs. 6.3%, p < 0.001). There was no significant difference in STEMI and non-STEMI group. The laboratory findings of blood parameters were shown in Table 3. Females had low hemoglobin (13.7 ± 2 vs. 11.7 ± 1.5, p < 0.001) and poor glycemic control (7.45 ± 1.9 vs. 8.06 ± 2.2, p < 0.001). The left ventricular function was given in Table 4.
Table 1Baseline characteristics of the 1,595 patients in the study
Total no of patients: 1,595
Male: 1,293
Female: 302
p-Value
Age, mean (SD), years
58.2 ± 10.8
58 ± 10.9
60.8 ± 9.1
<0.001
Height, mean (SD)
162.6 ± 8.3
164.6 ± 7.5
154 ± 7.3
<0.001
BMI, mean (SD)
26.3 ± 6.2
26.2 ± 6.7
27.2 ± 4
<0.001
Diabetes mellitus (%)
957 (60)
747(57.8)
210 (69.5)
<0.001
Hypertension (%)
845 (53)
649(50.2)
196 (65)
<0.001
Dyslipidemia (%)
273 (17)
215 (16.7)
58 (19.3)
0.3
Smoker (%)
99 (6.2)
99(7.7)
0
<0.001
Alcoholic (%)
91 (5.7)
90 (7)
1 (0.3)
<0.001
Family history of CAD (%)
240 (15)
204 (15.8)
36 (12)
0.1
CVA (%)
34 (2.1)
29 (2.2)
5 (1.7)
0.6
COPD (%)
5 (0.3)
5 (0.4)
0
0.6
CKD (%)
49 (3.1)
47 (3.6)
2 (0.7)
0.005
K/C/O CAD (%)
471 (29.5)
390 (30.2)
81(27)
0.3
H/O PCI (%)
232 (14.5)
190 (14.7)
42 (14)
0.9
H/O CABG (%)
94 (5.9)
82 (6.3)
12 (4)
0.1
Clinical presentation
Unstable angina (%)
277 (17.4)
209 (16.2)
68 (22.7)
0.009
MI < 90 days (%)
513 (32.2)
434 (33.6)
79 (26.3)
0.02
Thrombolysis (%)
196 (12.1)
174 (13.5%)
19 (6.3%)
< 0.001
NSTEMI (%)
298 (18.7)
236 (18.3%)
62 (20.5%)
0.4
STEMI (%)
381 (23.8)
310 (24%)
71 (23.5%)
0.9
Total no of patients: 1, 595
Male: 1,293
Female: 302
p-Value
Hemoglobin, mean (SD), g/dL
13.3 (2.1)
13.7 (2)
11.7 (1.52)
<0.001
Urea, mean (SD), mg/dL
26.2 (11.9)
26.4 (11.6)
25.1(9.8)
0.4
Creatinine, mean (SD), mg/dL
0.9 (0.5)
0.9 (0.6)
0.7 (0.3)
0.9
HbA1c, mean (SD), mg/dL
7.5 (2)
7.45 (1.9)
8.06 (2.24)
<0.001
Total no of patients: 1,595
Male: 1,293
Female: 302
p-Value
LVEF ≤45 (%)
949 (59.5)
782 (60.5%)
167 (55.6%)
0.1
LVEF > 45 (%)
646 (40.5)
511 (39.5%)
135 (45%)
Table 4Procedural characteristics
Total no of patients: 1,595
Male: 1,293
Female: 302
p-Value
Systolic BP mm Hg, mean (SD)
140.6 (24.6)
139.7 (24.5)
146.5(25.7)
<0.001
Diastolic BP mm Hg, mean (SD)
78.4 (13.5)
79.1 (13.9)
75.6 (11.9)
0.001
TPI (%)
32 (2)
23 (1.8%)
9 (3%)
0.2
IABP (%)
83 (5.2)
75 (5.8%)
8 (2.6%)
0.03
GpIIb/IIIa (%)
198 (12.4)
160 (12.4%)
38 (12.6%)
0.9
Heparin (%)
1336 (83.7)
1072 (83%)
264 (87.7%)
0.04
Bivalirudin (%)
255 (116)
220 (17%)
35 (11.6%)
0.02
Sex Difference in Procedural CharacteristicsThe procedural and angiographic characteristics were reported in Tables 5 and 6. Intraaortic balloon pump usage was more in men (5.8 vs. 2.6%, p-0.03). There was no significant difference in vessels involved or the total number of lesions. Femoral access (53.6 vs. 65.3%, p < 0.001) was most preferred access for females as radial access (44.8 vs. 33.4%, p < 0.001) in men.
Table 5Angiographic data of 1,595 patients; male versus female
Disease
Total no of patients: 1,595
Male: 1,293
Female: 302
p -Value
SVD (%)
1225 (76.8)
999 (77.2)
226 (74.8)
0.4
DVD (%)
334 (21)
265 (20.5)
69 (22.8)
0.4
TVD (%)
36 (2.3)
29 (2.2)
7 (2.3)
1
Vessel involved
Total no of lesions: 1,983
Male: 1,616
Female: 367
p -Value
LAD (%)
957 (48.2)
767 (47.4)
190(51.7)
0.1
LCX (%)
385 (19.4)
322 (20)
63(17.1)
0.1
RCA (%)
549 (27.7)
455 (28.1)
94(25.6)
0.2
LM (%)
28 (1.4)
19 (1.2)
9 (2.5)
0.09
ISR (%)
32 (1.6)
23 (1.4)
9(2.5)
0.3
SVG (%)
32 (1.6)
30 (1.9)
2(0.5)
0.07
Access
Total no of patients: 1,595
Male: 1,293
Female: 302
p -Value
Brachial artery (%)
1 (0.06)
1 (0.1%)
0
<0.001
Dorsoradial (%)
12 (0.8)
12 (0.9%)
0
Femoral artery (%)
889 (55.7)
693 (53.6%)
196 (65.3%)
Radial artery (%)
680 (43)
579 (44.8%)
101 (33.4%)
Radial and femoral (%)
13 (0.8)
8 (0.6%)
5 (1.7%)
Table 6In-hospital clinical outcomes between male and female patients
Total no of patients: 1,595
Male: 1,293
Female: 302
p-Value
Hospital stay, mean (SD), days
4 (2.2)
3.9 (2.2)
4 (2.3)
0.2
Mortality (%)
19 (1.2)
16 (1.2)
3 (1)
1
Minor and major bleeding (%)
29 (1.8)
17 (1.3)
12 (4)
0.006
Stroke (%)
9 (0.6)
8 (0.6)
1 (0.4)
1
Repeat revascularization (%)
6 (0.4)
4 (0.2)
2 (0.6)
0.3
Reinfarction (%)
9 (0.6)
5 (0.4)
2 (0.6)
0.6
Sex Difference in Clinical OutcomesIn-hospital clinical outcomes were shown in Table 6. The bleeding complications were high in the female group (1.3 vs. 4%, p-0.006). There were no significant differences in in-hospital mortality and other MACE events.
DiscussionOur study showed that women admitted for PCI were on an average of 2.8 years older than men that is inconsistent with previous studies published.14 15 This could be due to the protective role of circulating estrogens in younger women. The cardioprotective actions of estrogen are vasodilatation, reduced reactive oxidative stress, and fibrosis.16
DM and HTN were more prevalent in women when compared with men. Even though DM might affect men and women equally females are highly impacted by its consequences. Premenopausal diabetic women lose protection against heart disease.17 A study also reported that the diabetic women who presented with ACS had 36.9% mortality when compared with euglycemic women presenting with ACS 20.2%.18 Women aged ≥55 years have a higher prevalence of HTN than men, indicating the loss of arterial elasticity.19 20 Endogenous estrogens maintain vasodilation and contribute to blood pressure control in premenopausal women.21 During the menopause transition, the rise in systolic blood pressure is due to a decline in estrogen levels. Postmenopause, there is an upregulation of the renin-angiotensin system and increased plasma renin activity.22 With higher systolic blood pressure, the risk of coronary heart disease increases. Systolic blood pressure of at least 140 mm Hg increases coronary heart disease risk by 37% and for stroke by 86% in women.23
Increasing body weight is associated with increased coronary risk and fourfold increased risk in cardiovascular events in the heaviest category women compared with lean women.24
Few studies reported that truncal obesity and increased BMI as independent risk factors in young female patients with coronary artery disease (CAD). For predicting premature CAD, the sagittal abdominal diameter to skin fold ratio seems to be a good indicator.25
Clinical presentation of ACS differs between men and women. Women commonly presented with unstable angina compared with men.
From “bench to beyond premature ACS” study, irrespective of the type of ACS, chest pain is the most prevalent symptom among both sexes. However, women were more likely to present with diverse symptoms.26 They generally present with pain in the upper back, arm, neck, or jaw, and also as indigestion, nausea, vomiting, and palpitations. Shoulder pain and arm pain are twice as predictive of an ACS diagnosis in women compared with men27
The rate of thrombolysis is also less among women in our study. In a pooled analysis of 22 trials, 6,763 STEMI patients were randomized to primary PCI versus thrombolytic and found that women had lower 30-day mortality in primary PCI regardless of the time of presentation.28 Because of multiple relative contraindications for thrombolysis in women, treating physicians are reluctant to use thrombolytic therapy for STEMI in women.2 Another important observation in our study is that bleeding rates are higher among females. GUTSO-I trial reported that bleeding risk increased by 1.43-fold in women and showed higher risk of bleeding complications.29
The mortality due to CVD is the leading cause of death in women worldwide and higher among women when compared with men30 there is no significant difference in mortality noted in our study, perhaps due to the inequality in sample size. Kerala ACS registry also showed among 25,748 ACS patients, 5,825 were women, and there was no difference in the outcome of death, reinfarction, or stroke between both genders.31 Detection and management of coronary heart disease (DEMAT) registry also showed similar results.32
Though there is no significant mortality difference, bleeding events are significantly higher in women in our study that is consistent with other studies. Higher rates of bleeding after MI are seen in women than men.33 Global Registry of Acute Coronary Events (GRACE) trial showed that bleeding risk increased by 43% in women during hospitalization. PCI in women showed a significantly higher incidence of in-hospital major bleeding in other studies34 35
ConclusionOur single-center study among patients undergoing PCI showed that women with ACS present at a later age compared with men and have a higher prevalence of risk factors like DM and HTN. Though there is no gender-based difference in in-hospital mortality after PCI, women have an increased risk of bleeding. Larger studies are needed to confirm this study's findings.
Appendix A: Thrombolysis in myocardial infarction (TIMI) bleeding criteria11Major
Any intracranial bleeding excluding microhemorrhage <10 mm that is evident only on gradient-echo magnetic resonance imaging (MRI).
Clinically overt signs of hemorrhage associated with a hemoglobin drop of 5 g/dL.
Fatal bleeding which results in death within 7 days.
Minor:
Resulting in hemoglobin drop of 3 to <5 g/dL or 10% decrease in hematocrit.
Any overt sign of hemorrhage that meets any one of the following criteria and does not meet criteria for a major or minor bleeding event, as mentioned above.
Minimal:
Appendix B: Definition of clinical events
Clinical events
ST elevation12
New ST elevation at the J point in more than two contiguous leads with greater than or equal to 0.2 mV in lead V1, V2, or V3 and 0.1 mV in other leads
MACCE 12
Composite of death, nonfatal myocardial infarction, stroke
Death12
Patient died during hospitalization/ documentation of death during follow-up
Myocardial infarction12
Increase in cardiac biomarker values preferably cardiac troponin with at least one value above the 99th percentile URL and with at least any one of the following criteria with
(i) symptoms of ischemia, (ii) new significant ST segment–T wave (ST–T) changes or new LBBB, (iii) onset of pathological Q waves in the electrocardiogram, or (iv) new findings of non-viable myocardium or new regional wall motion abnormality in imaging, (v) presence of an intracoronary thrombus either by angiography or autopsy
Stroke12
Loss of neurological function caused by an ischemic or hemorrhagic event with residual symptoms at least 24h after onset or leading to death
Cardiogenic shock12
A systolic blood pressure of less than 90 mm Hg for at least 30 minutes or when need of any supportive measures to maintain a systolic blood pressure of more than 90 mm Hg. End-organ hypoperfusion is when the extremities are cold or when the urine output is less than 30 mL/h, and a heart rate is greater than or equal to 60 beats per minute
PCI—clinically driven target lesion revascularization13
PCI–TLR is when the target lesion diameter stenosis is >50% by QCA and the subject has clinical or functional ischemia that cannot be explained by another native coronary or bypass graft lesion. Even with absence of the above signs or symptoms if when there is >70% diameter stenosis in QCA, it is considered as significant. When QCA data are not available or when there is > 50% stenosis, in presence of severe ischemic signs and symptoms attributed to the target lesion
Abbreviations: LBBB, left bundle branch block; MACCE, major adverse cardio and cerebrovascular event; PCI-TLR, percutaneous coronary intervention-target lesion revascularization; QCA, quantitative coronary angiography.
Comments (0)